Spotlight On Dentistry: Can’t you just scrape that off his teeth?
February is Pet Dental Health Month and at Veterinary General we feel dental health is crucial to the overall health of your pet. Volumes of books can and have been written on dentistry but in this entry we are going to look at each step in the cleaning process and explain why they are important. Since advanced periodontal disease and treatment is beyond the scope of this article we will only look at the cleaning details of a patient undergoing a “Stage 1” (see Initial Evaluation below) dental cleaning.
Dental care is quickly evolving in veterinary medicine and old recommendations are being discarded in light of research. It is not uncommon to get questions about dental radiographs, pre-anesthetic blood work, home care, and why those items are even important in a younger dog with mild tartar. Cost is another concern, and we often have clients compare costs from previous pets or other practices. Through education we hope to share the value of the complete dental prophylaxis and show how it is not just simply “cleaning the teeth.”
Initial Evaluation
The dental therapy process begins with an oral examination of the pet. The veterinarian or veterinary technician will stage a pet’s teeth based upon amount of tartar and gum irritation visible. This visual inspection allows us to create and plan and estimated cost for the procedure. Pets with more severe periodontal disease require more advance treatments and are discussed on an individual basis.
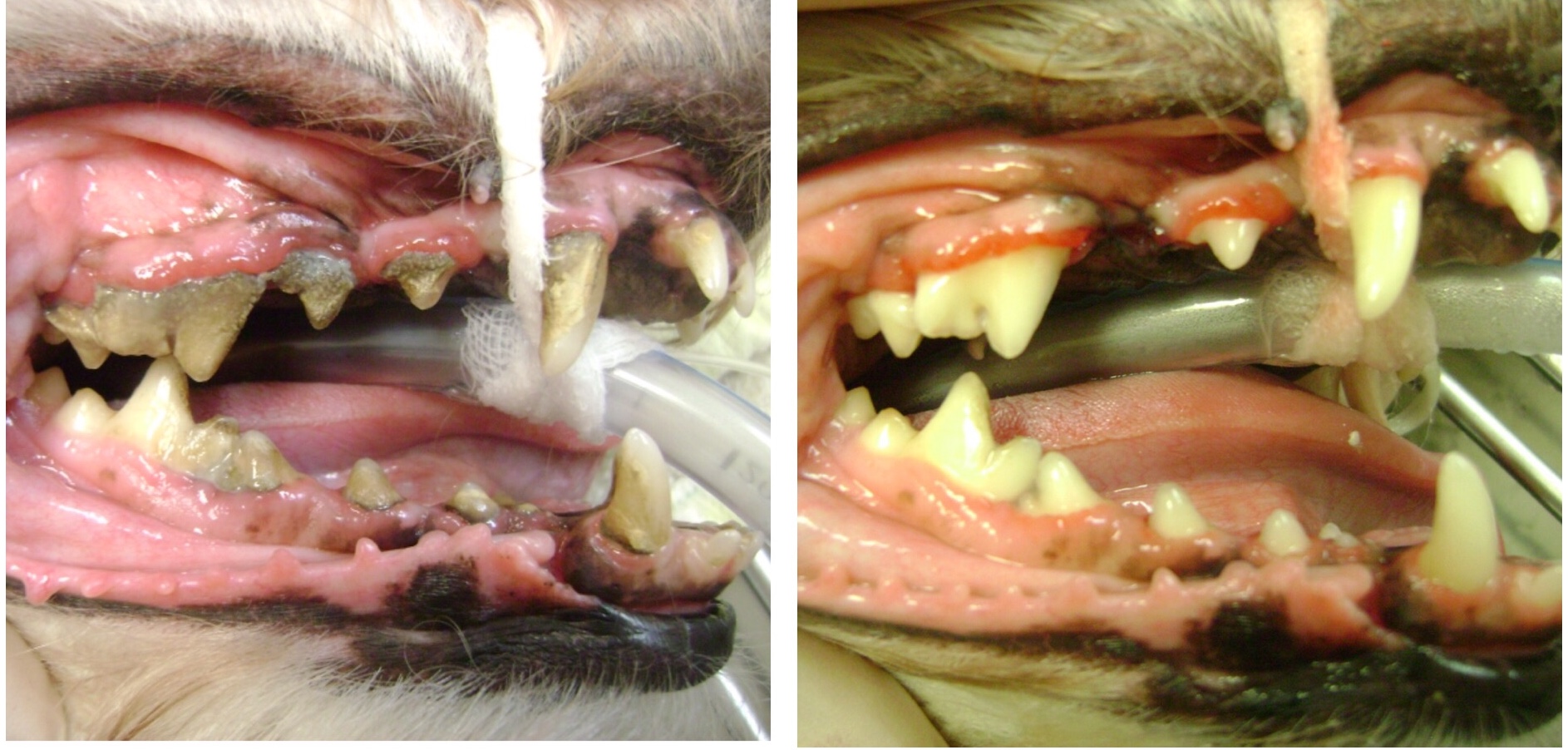
Dental disease is “staged” from one through four, with four being most severe. Stage one dental disease is marked by halitosis (bad breath), mild calculus (tartar) build up, inflamed and red gum line. In stage two there is more calculus build up, the gum line will appear shiny, and swollen. Stage three is marked by swelling and recession of the gum line that may bleed with gentle probing. Stage four is identified by severe inflammation, pain, gum recession, bleeding, and purulent (pus) discharge. These are simply the visible signs, a more accurate assessment is made when dental radiographs and charting are completed (VetMed Team).
Blood Work and Anesthesia
Pre-anesthetic blood work is required for all patients receiving a dental cleaning. The liver and kidneys are responsible for converting drugs into a form the body can use then removing them from the body. If the liver and kidneys are not functioning properly the anesthetic protocol can be altered or the procedure aborted. Dental disease can cause changes in the rest of the body and blood work will help us identify any potential problems.
During anesthesia the patient is monitored by a licensed veterinary technician at all times. Monitoring includes heart rate, respiratory rate, temperature, percent of oxygen in the blood, and blood pressure. All patients have IV catheters placed, receive IV fluids during the procedure, and have endotracheal tubes placed in their trachea. IV fluids help maintain blood pressure during anesthesia and allow for injections to be given if needed. Endotracheal tubes have a small balloon on the end that can be inflated to prevent fluid from entering the lungs.
Dental Radiographs
The veterinary technician begins the dental process with radiographs. Radiographs are key component between a complete dental prophylaxis and just cleaning the teeth. Cleaning and observing abnormalities above the gum line ignores 60% of the tooth (Iams Partners for Health, 2003). Radiographs allow the veterinarian to evaluate the root of a tooth, bone loss around the root, and pockets (spaces between the gum and tooth root). If caries (cavities in people) is seen on the surface of the tooth a radiograph will allow the veterinarian to assess how far the lesion affects the tooth. After extractions an x-ray is often taking to make sure the entire root of a tooth has been extracted. Radiographs can also reveal roots of baby teeth that did not fall out, and adult teeth that never erupted through the gum line.
Charting
The first step with charting is a second oral exam. This allows the veterinary technician to note any abnormalities that were not observable on the patient while awake. Pictures are taken for both the patient’s records and the pet’s owners. The veterinary technician then begins to chart the oral cavity. They insert an instrument, called a probe, gently between the tooth and gums. A small depth is acceptable and requires no treatment however; bigger “pockets” need attention and indicate periodontal disease. The technician will also note any missing, fractured, discolored, or loose teeth.
Charting and dental radiographs are the foundation of the veterinarian’s treatment plan (VetMed Team). A treatment plan will include a diagnosis, recommendations for treatment (including extractions if needed), prognosis, and home care plan.
Dental Cleaning, Polishing, and Fluoride Treatment
Cleaning begins by removing large pieces of tartar by hand scaling both above and below the gum line. Ultrasonic scaling will be used to remove any material that was left behind. Once again the mouth is visibly inspected for any remaining tartar, and a probe is run over the tooth to “feel” for any irregularities caused by tartar left on the tooth (VetMed Team).
After scaling is complete the teeth are then polished. Scaling can create micro abrasions on the tooth’s surface. If these abrasions are not smoothed out, they will provide a foothold for plaque and tartar formation. Finally the mouth is rinsed with water, to flush out any debris, and air dried. A fluoride treatment is applied to the teeth to strengthen the enamel.
Home Care
The true definition of prophylaxis is “the prevention of disease or control of its possible spread (Farlex).” A dental cleaning is a treatment of a disease process, whereas true prophylaxis is done at home. Home therapy is targeted at removing or lowering the amount of bacteria in the mouth. If home care is not instituted by three months after a dental cleaning then gingivitis scores are equivalent to those recorded prior to dental cleaning (Gorrel, 2004).
Brushing teeth is the gold standard for at home dental care; however, there are many options available. Products range from traditional tooth paste and tooth brush, to toys, treats, chews, wipes, and sprays. This allows us to design the home care plan that fits your pet’s needs and your lifestyle as well. Home care is a large subject matter and will be the focus of a later blog.
Conclusion
True dental prophylaxis encompasses both the professional dental cleaning under anesthesia coupled with home care. Dental cleanings that are incomplete or focus on the visible tooth anatomy can regress quickly. To answer my opening question; No, we cannot just simply scrape that off his teeth.
Works Cited
Farlex. (n.d.). The Free Dictionary. Retrieved February 1, 2013, from http://www.thefreedictionary.com/prophylaxis
Gorrel, C. (2004). Veterinary Denistry for the General Practitioner. Edinburgh, London, NY, Oxford, Philadelphia,St. Louis, Sydney, Toronoto: Saunders.
Iams Partners for Health. (2003). Spotlight on Dentistry: More than meets the eye.
VetMed Team. (n.d.). Companion Animal Denistry 101. Retrieved January 20, 2013, from www.vetmedlearn.com
VetMed Team. (n.d.). Companion Animal Dentistry 102. Retrieved January 20, 2013, from www.vetmedlearn.com










Recent Comments