Spotlight On Parasitology: Heartworm Disease
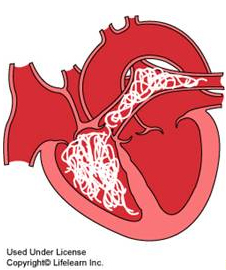
Everyone knows their dog needs yearly heartworm preventative, but do they really know what heartworm is or why we give preventatives? Heartworm disease is caused by parasitic worms that make their home in the arteries leading to the lungs and sometimes in the right side of the heart. These parasites can infect dogs, cats, wolves, foxes, ferrets, and sea lions (American Heartworm Society, 2013). Though rare, humans can also be infected by heartworm larva. The immature heartworms don’t survive long in humans, but they end up in the lungs causing nodules to form (CAPC, 2009). These nodules can be mistaken for tumors or tuberculosis!
Life Cycle and Stages
The lifecycle of the heartworm involves numerous steps before they mature into adult heartworm. Adult heartworms live the arteries between the heart and lungs, where females give birth to live young, called microfilaria. Microfilaria must be ingested by a mosquito before they become infectious. This means heartworm cannot be from pet-to-pet contact, it can only be transmitted by mosquitoes. Dogs are highly susceptible to infection, virtually 100% of dogs exposed become infected, whereas 61-90% of cats become infected (American Heartworm Society, 2013). After entering the pet the adolescent worms spend up to 70 days migrating through the tissues of the body before they make their way into the bloodstream.
Where is it found?
Heartworm disease is found worldwide and in all 50 states. It is found in higher numbers in warm, moist climates. The Southeastern United States and the Mississippi River Valley have the greatest number of reported cases in the US (CAPC, 2009). Michigan comes in with an average of 6-25 cases per clinic. Please keep in mind the actual number may be higher as these numbers are reported cases, and not all veterinary clinics report positive cases.
Clinical Signs and Testing
In the early stages of heartworm disease the clinical signs are mild and can even be absent. Dogs suffering from severe heartworm disease may have a persistent cough, exercise intolerance, abnormal lung sounds, fluid in the chest cavity, episodes of passing out, and/or weight loss. Dogs can harbor 30 or more adult heartworms; this large number of worms can alter blood flow through the heart and potentially interfere the normal function of the heart. This can cause the heart to work harder to pump blood throughout the body, and can lead to murmurs, severe heart disease, anemia, and more (CAPC, 2009).
Testing for dogs is very simple and looks for the presence of a protein found only on the surface of female heartworms. For dogs that return positive a confirmatory test is performed to rule out any potential false positive results. If both tests are positive the dog is considered heartworm positive.
Cats with heartworm disease display symptoms similar to feline asthma, bronchitis, or can have no symptoms at all (American Heartworm Society, 2013). Symptoms include vomiting, coughing, difficulty breathing, diarrhea, and not eating. Anyone who has owned a cat can tell you that not eating and vomiting can be a regular occurrence in their cat, thus making the heartworm diagnosis more difficult.
Testing for cats is different because cats have smaller hearts than dogs therefore usually harbor only 1-2 adult heartworms. Heartworm test for cats looks for the body’s immune system response to the heartworms rather than an antigen testing used in dogs.
Treatment
Heartworm disease is treatable in dogs; however it can be costly and recovery is very lengthy. Treatment is designed to kill off circulating microfilaria (immature heartworm) and adult heartworms while minimizing complications caused by worm die off and treatment. The dog undergoing treatment should be as healthy as possible before undergoing treatment (AHS, 2013). Treatment consists of three injections of melarsomine, derived from arsenic, over 31 days (Think 12, AHS, 2012). To reduce side effects and complications of treatment an antibiotics, steroids, and medications to control heart disease may also be prescribed. Dogs with severe heartworm disease may require surgical removal of the heartworms.
During and after treatment, dogs are on a very strict exercise regimen. All excitement and exercise (beyond slow walking for bathroom breaks) should be restricted. As the worms die off and begin to decompose they can become lodged in arteries and capillaries around the heart and lungs. Increased activity causes more blood to flow to these blocked vessels and increase risk of cardiovascular side effects including heart failure (AHS, 2013).
Unfortunately there is no approved treatment for heartworm disease in cats (American Heartworm Society, 2013). Cats react severely when the worms begin to die off. This reaction can cause shock and even death. In some cases surgical removal of the adult heartworms may be attempted.
Next time we will look at heartworm preventatives.
Works Cited
AHS. (2013). Canine Guidelines. Retrieved February 8, 2013, from American Heartworm Society: www.heartwormsociety.org/veterinary-resources/canine-guidelines-summary.html
American Heartworm Society. (2013). What is Heartworm Disease? Retrieved February 8, 2013, from www.heartwormsociety.org/pet-owner-resources/heartworm.html
CAPC. (2009, November). Canine Heartworm CAPC Vet. Retrieved February 8, 2013, from Companion Animal Parasite Council: www.capcvet.org/capc-recommendations/canine-heartworm
Think 12, AHS. (2012). Think 12. Retrieved February 8, 2013, from Truth About Treatment, Mosquitos in Winter, Don’t Try to Predict-Protect: http://www.heartwormsociety.org/think12/












Recent Comments